
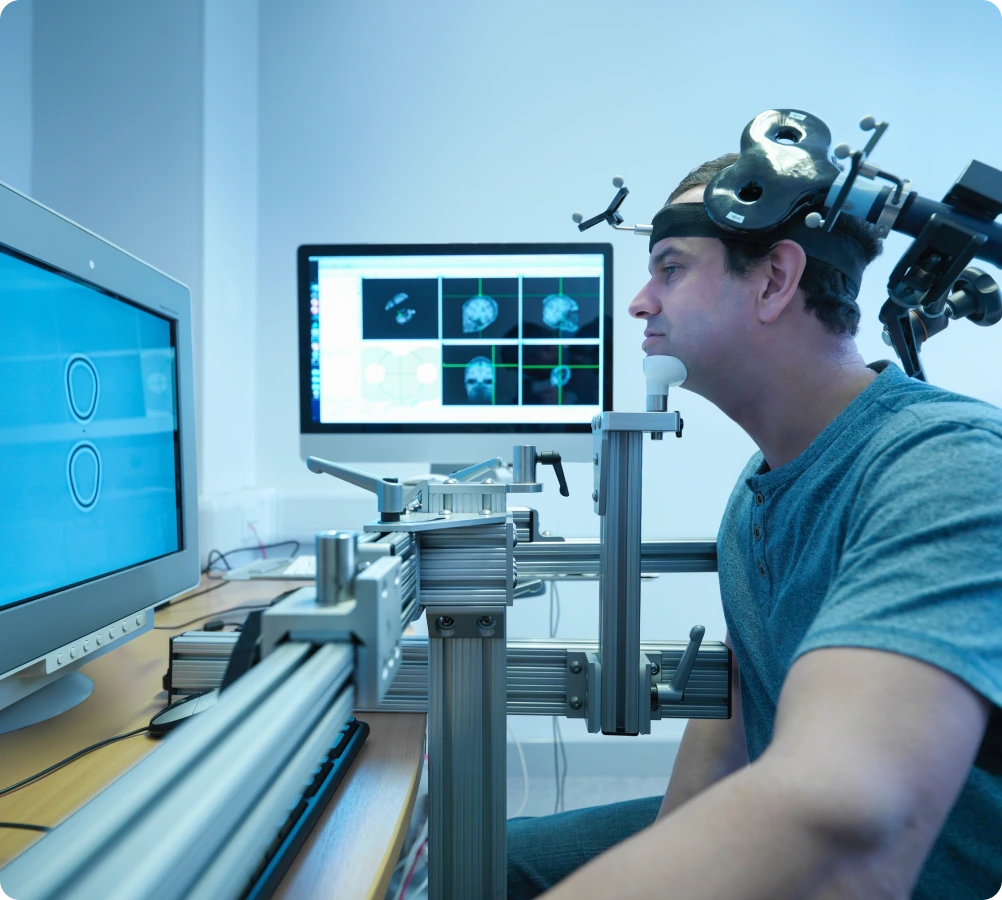
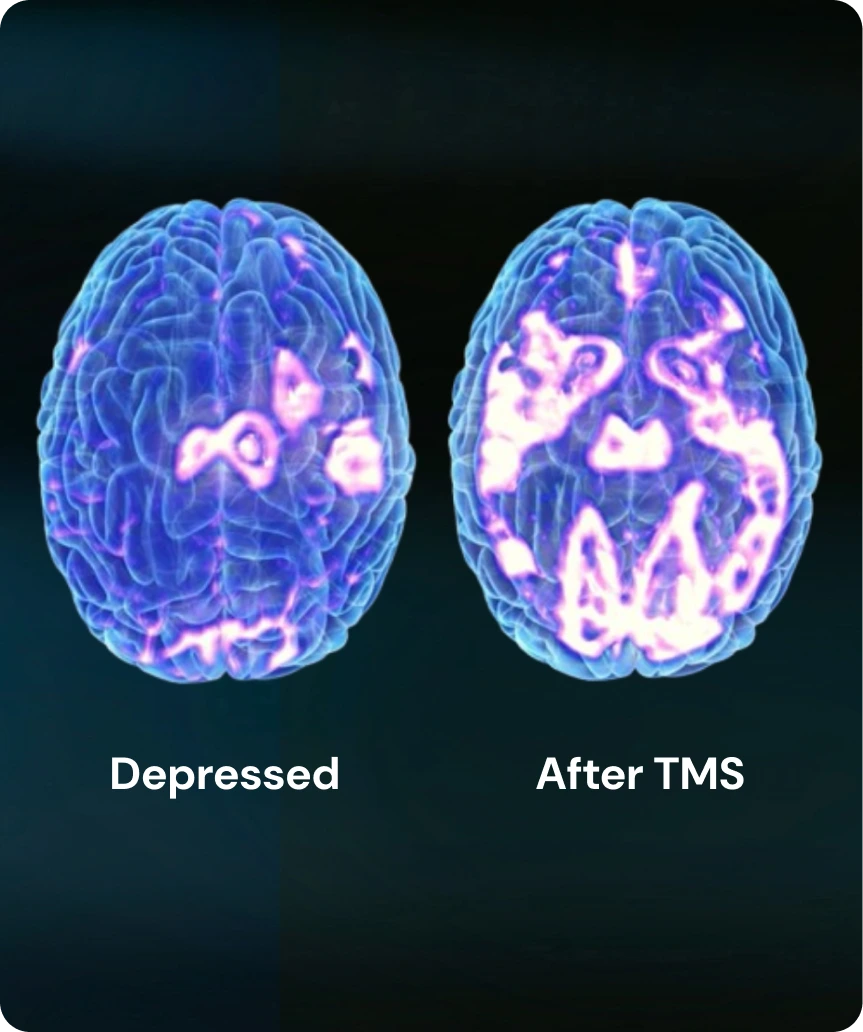
Transcranial magnetic stimulation (TMS) therapy is a non-invasive, FDA-approved treatment for major depressive disorder that uses electromagnetic pulses to stimulate nerve cells involved in mood regulation. During this procedure, a therapist places a magnetic coil against the patient’s scalp near the forehead and delivers precise signals in a repetitive, painless manner.

Side Effects
Results
Long-Term Maintenance
Failed Medication Treatment
People who have failed to achieve remission after trying several antidepressant medications are the main candidates... for TMS therapy. Our treatment can address the problem and help achieve mental wellness.
Read moreUnable to Tolerate Medication Side Effects
Some people are unable to tolerate the side effects of antidepressant medications, even after trying several different drugs.... They can benefit from brain stimulation, which is much milder than SSRIs and antipsychotics. TMS therapy is a non-invasive treatment without significant complications. Patients may only experience mild headaches initially, but they gradually disappear.
Read moreWant to Avoid
Drugs
Want to Avoid Drugs
Some people prefer to avoid psychiatric medication if possible. This category of patients is less common, yet they may... still benefit from brain stimulation. TMS therapy can be an excellent option for such patients because it does not involve taking any pills or substances.
Read morePregnant Women With Depression
Women dealing with prenatal or postpartum depression have limited treatment options, as many antidepressant... drugs pose risks during pregnancy and breastfeeding. For these patients with special contraindications, TMS offers a drug-free approach to managing their mental health that can be safer for mom and baby. We recommend discussing this issue with a therapist to determine the most suitable treatment protocol.
Read more