TMS for Brain Injury: Restoring Memory, Mood, and Cognitive Function
TMS therapy is a non-invasive treatment option gaining attention for individuals recovering from brain injuries who struggle with lingering cognitive, emotional, or neurological symptoms. Many patients experience challenges, such as persistent headaches, mood changes, memory issues, or difficulty concentrating, which can make daily life and rehabilitation frustrating. TMS offers a targeted approach to stimulate neural activity, potentially improving cognitive function, mood, and overall quality of life.
At TMS Therapy Near Me, we make it easy to connect with qualified TMS providers across the U.S., helping you find the right specialist near you to explore whether this therapy could be a beneficial part of your recovery journey.
TMS for Brain Injury: Restoring Memory, Mood, and Cognitive Function
TMS therapy is a non-invasive treatment option gaining attention for individuals recovering from brain injuries who struggle with lingering cognitive, emotional, or neurological symptoms. Many patients experience challenges, such as persistent headaches, mood changes, memory issues, or difficulty concentrating, which can make daily life and rehabilitation frustrating. TMS offers a targeted approach to stimulate neural activity, potentially improving cognitive function, mood, and overall quality of life.
At TMS Therapy Near Me, we make it easy to connect with qualified TMS providers across the U.S., helping you find the right specialist near you to explore whether this therapy could be a beneficial part of your recovery journey.

What Is TMS?
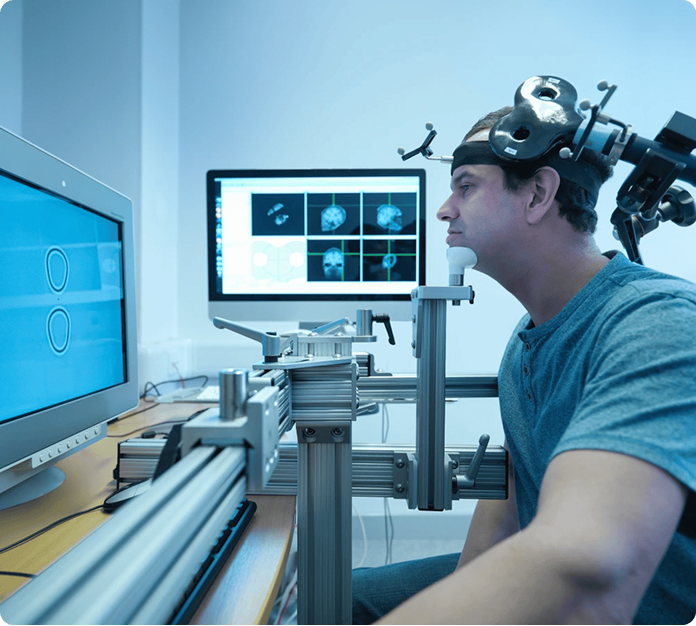
Transcranial magnetic stimulation (TMS) is a non-invasive therapy that uses magnetic pulses to stimulate specific areas of the brain. It’s designed to help regulate brain activity and support recovery from conditions like depression, cognitive challenges, and symptoms related to brain injury. Unlike medications or surgery, TMS is outpatient, painless, and does not require anesthesia, making it a convenient option for those seeking targeted, evidence-based brain therapy.
TMS for Brain Injury
TMS is an emerging treatment option for individuals dealing with the lasting effects of traumatic brain injury (TBI) or other forms of head trauma. Research suggests that TMS may help support the recovery of brain function by stimulating neural pathways that have been disrupted by injury. This can be particularly valuable for patients with diffuse axonal injury, a type of brain damage that affects communication between brain regions. While results can vary, many patients pursue TMS to improve cognitive performance, mood, and overall quality of life after a brain injury.
What to Expect During Your Appointments
Consultation
The TMS journey begins with a thorough consultation with a licensed provider, where your medical history, symptoms, and prior treatments are reviewed. This step helps determine whether TMS is a suitable option for your specific brain injury needs. The provider will discuss potential benefits, risks, and what to expect during treatment, helping you make an informed decision about pursuing therapy.
Brain Mapping
Before treatment begins, a process called brain mapping is performed to identify specific brain regions to target with TMS. This ensures that the magnetic pulses are delivered precisely to areas most relevant for your symptoms. Brain mapping is tailored to each patient, taking into account the unique pattern of injury and the brain’s individual anatomy.
Determining Motor Threshold
Next, your motor threshold is measured, which is the minimum level of magnetic stimulation required to produce a response in a specific muscle. This measurement ensures that the treatment intensity is personalized for safety and effectiveness, allowing the provider to stimulate the brain accurately without causing discomfort.
TMS Treatment Sessions
During TMS sessions, an electromagnetic coil is placed against the scalp to deliver short magnetic pulses to the targeted brain regions. These pulses penetrate the skull and influence neural activity, encouraging cortical plasticity, or the brain’s ability to reorganize and form new connections. Sessions typically last 3–40 minutes and are non-invasive, with patients fully awake and alert throughout.
Follow-Up and Monitoring
Throughout TMS therapy, progress is closely monitored to assess symptom changes and adjust treatment as needed. Follow-up sessions help ensure that stimulation is optimized and that the patient experiences maximum benefit while minimizing side effects.

Recovery & Side Effects
After TMS treatment for brain injury, many patients notice gradual improvements in cognitive function, mood, and overall daily performance as brain activity in targeted areas begins to normalize. Recovery is typically smooth, with most people able to resume normal activities immediately after each session. Some mild side effects may occur, including temporary scalp discomfort or facial muscle twitching, but these usually resolve quickly and are well-tolerated. Regular monitoring by your provider ensures that any discomfort is managed and that therapy continues safely throughout treatment.
Candidates for TMS for Brain Injury
Mild Traumatic Brain Injury
Individuals with mild traumatic brain injury may benefit from TMS if they experience persistent postconcussion symptoms, such as difficulty concentrating, memory problems, or mild headaches. TMS can help support neural recovery and improve overall cognitive function in these patients.
Severe Traumatic Brain Injury
Patients recovering from severe traumatic brain injury may use TMS to aid in restoring motor functions, cognitive abilities, and mood. TMS can sometimes complement traditional rehabilitation therapies, especially for those who have plateaued in recovery through conventional methods.
Stroke and Cerebral Ischemia
Stroke patients or those who have experienced cerebral ischemia may be candidates for TMS to help stimulate affected brain regions, support cortical plasticity, and improve motor or cognitive deficits, depending on the severity and location of the injury.
Acute Phase and Coma Recovery
TMS is generally not applied during the acute phase of brain injury, but patients emerging from coma recovery may be evaluated for therapy to support early neural rehabilitation once medically stable.
Special Considerations
Certain conditions may limit TMS use. Patients with cochlear implants or magnetic-sensitive metal implants within 12 inches of the treatment site may not be eligible due to safety risks associated with magnetic pulses. A thorough medical review ensures that TMS is both safe and appropriate for each individual.

Benefits of TMS for Brain Injury
- Non-invasive therapy with no need for anesthesia
- Can improve cognitive function, memory, and attention after brain injury
- May help restore motor functions affected by trauma or stroke
- Supports recovery from mood changes, depression, and anxiety linked to brain injury
- Promotes cortical plasticity, encouraging the brain to form new neural connections
- Reduces persistent postconcussion symptoms, including headaches
Cost of TMS for Brain Injury in the U.S.
The cost of TMS for brain injury in the U.S. typically ranges from $100 to $300 per session without insurance. Total treatment costs can vary depending on the number of sessions prescribed, the provider’s location, and any additional evaluations or mapping procedures. While some insurance plans may cover TMS for related conditions, it’s important to check with your provider and insurance company beforehand to understand potential out-of-pocket expenses.

Try Our Noninvasive Brain Stimulation Techniques
Explore a range of non-invasive brain stimulation options designed to support recovery and improve quality of life for individuals with head injuries or other neurological conditions. These therapies have shown promise for patients dealing with post-concussion symptoms, frequent headaches, and central pain, helping to reduce discomfort and enhance daily functioning. In addition, research indicates improvements in working memory, and TMS may also complement treatment for major depressive disorder in patients whose mood changes follow brain injury. Non-invasive brain stimulation offers a safe approach for addressing both the physical and cognitive effects of head trauma.
Frequently Asked Questions (FAQ)
What is the difference between deep and repetitive transcranial magnetic stimulation (rTMS)?
Deep TMS penetrates deeper into the brain to stimulate broader networks, while high-frequency rTMS targets more superficial areas with repeated pulses. Studies show significant differences in the depth of stimulation and the range of neural circuits affected, which can influence treatment outcomes depending on the condition being treated.
Are there faster TMS protocols?
Yes, intermittent theta burst stimulation (iTBS) is a faster TMS protocol that delivers rapid bursts of magnetic pulses in a condensed session (3-9 minutes). This approach has been explored for patients with moderate and mild TBI to enhance recovery and strengthen neural connections more efficiently than standard TMS sessions.
How do magnetic pulses increase cortical excitability within the brain's motor cortex?
Magnetic pulses generate a rapidly changing magnetic field that penetrates the scalp and skull, inducing electrical currents in neurons. When applied to the primary motor cortex, these pulses can produce a motor-evoked potential and increase cerebral blood flow, enhancing the excitability of targeted neurons. TMS applied to other areas, such as the dorsolateral prefrontal cortex, works through similar mechanisms to modulate neural activity.
Is TMS safer than deep brain stimulation (DBS) and transcranial direct current stimulation (tDCS)?
TMS delivers targeted pulses of magnetic energy, while DBS is an invasive surgical procedure that implants electrodes in the brain. Compared with DBS, TMS is generally considered safer because it can modulate functional connectivity non-invasively, with minimal risk of permanent tissue damage or infection. Both tDCS and TMS are generally safe procedures, but TMS may offer more significant results.
What is diffusion tensor imaging, and how is it used in TMS therapy?
Diffusion tensor imaging (DTI) is an advanced MRI technique that maps white matter pathways in the brain. In TMS therapy, it helps identify regions of disrupted connectivity and track significant alterations in neural pathways, allowing clinicians to tailor treatment to improve clinical outcomes.
Can I combine TMS with other treatments?
Yes, TMS is often combined with medications or behavioral therapies. Research, including studies from Harvard Medical School, shows it can complement treatment for major depression, depressive symptoms, and obsessive-compulsive disorder. It can also be used alongside rehabilitation for severe TBI, targeting areas like the supplementary motor area to enhance motor and cognitive recovery.
Is TMS for TBI supported by randomized controlled trials and other clinical trials?
Yes, TMS for TBI has been studied in both placebo-controlled studies and trials using sham stimulation to measure effectiveness. Clinical trials have examined its impact on symptoms such as chronic pain and cognitive deficits by stimulating regions of the cerebral cortex, providing growing evidence for its safety and potential benefits.