Transcranial magnetic stimulation (TMS) therapy has emerged as a promising treatment option for individuals struggling with depression and other mental health conditions that have not responded to traditional approaches. As more patients consider this non-invasive alternative, one of the most common questions that arises is about the financial investment required. Understanding the cost of TMS therapy involves navigating a complex landscape of insurance coverage, treatment protocols, and regional pricing variations — factors that can significantly impact the overall expense for people seeking relief through this innovative treatment method.
Our online directory includes qualified TMS providers in your area, which could be a key to finding personalized support and relief.
TMS for Eating Disorders: A Non-Invasive Path to Neurological Balance
Our online directory includes qualified TMS providers in your area, which could be a key to finding personalized support and relief.

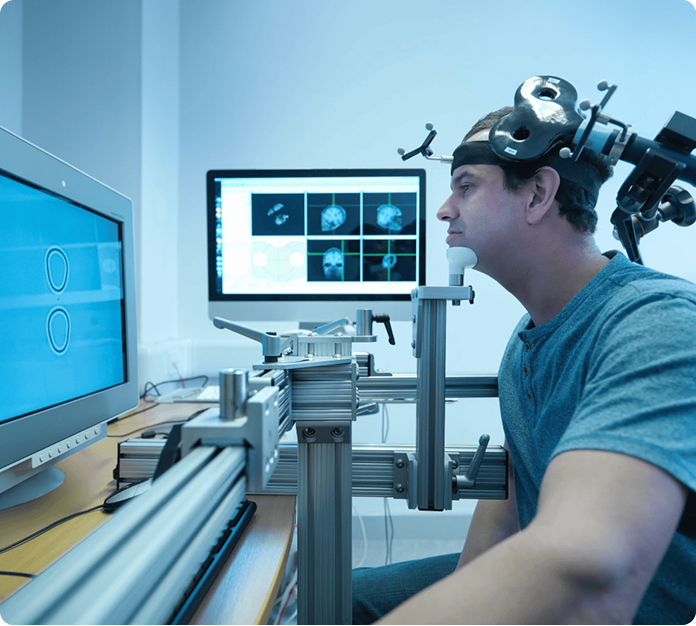
TMS is a non-invasive therapy that uses magnetic pulses to stimulate specific areas of the brain. It is designed to influence neural activity in regions involved in mood, behavior, and impulse control. TMS is FDA-cleared for certain mental health conditions and is increasingly being explored as a treatment for eating disorders.
Anorexia nervosa is characterized by extreme restriction of food, an intense fear of gaining weight, and a distorted body image. Patients often struggle with persistent thoughts about calories, weight, and control over eating, which can be difficult to manage through traditional therapy alone. TMS targets brain regions involved in mood regulation and impulse control, helping some individuals reduce anxiety around food and improve overall emotional balance.
Bulimia nervosa involves cycles of overeating followed by compensatory behaviors, such as self-induced vomiting, excessive exercise, or misuse of laxatives. Those affected often feel trapped by urges related to food intake and struggle with shame or guilt after binge episodes. TMS therapy may help by modulating brain activity associated with impulse control, reward processing, and emotional regulation, providing support alongside psychotherapy and nutritional guidance.
According to the National Eating Disorders Association, binge-eating disorder is marked by recurrent binge-eating episodes without regular compensatory behaviors. Individuals often experience feelings of loss of control, guilt, and distress after these episodes, which can significantly impact mental and physical health. TMS may offer relief by targeting brain circuits involved in craving, self-control, and mood regulation, helping patients gain more stability and reduce the frequency of binge-eating episodes.

Aftercare following TMS therapy typically involves ongoing check-ins with your provider to monitor progress and address any concerns as your treatment concludes. Most side effects are mild and temporary, such as scalp discomfort or headache, and serious side effects are rare. Some patients notice changes in appetite or eating patterns during recovery, which may include concerns about weight gain or shifts in cravings toward tasty yet unhealthy foods. Providers emphasize continued support, nutrition guidance, and therapy to help patients navigate these changes in a healthy, balanced way.

The cost of TMS for eating disorders in the U.S. typically ranges from $100 to $300 per session without insurance, depending on the provider, location, and treatment protocol. While coverage for eating disorder treatment varies, many clinics offer flexible payment plans and transparent pricing to make care more accessible. As research expands and more providers offer TMS, this therapy is becoming increasingly affordable, giving patients more options to pursue brain-based treatment closer to home.
